Article by: Renee Sorrentino, MD
Paraphilic disorders are rarely part of the curriculum for psychiatry residents or fellows. As a result, there are few psychiatrists who work with individuals who have paraphilic disorders.
In the past few decades, research on sexual offenders has shown that those with paraphilic disorders are at high risk for committing future sexual offenses. Psychiatrists can serve a pivotal role in reducing sexual offender recidivism by treating individuals with paraphilic disorders.
DSM overview
DSM originally characterized sexual deviations with psychopathic personality disorders based on the belief that sexual deviations were criminal acts, and thereby those individuals who engaged in sexual deviations were unlawful or psychopathic. DSM-II defined sexual deviations in a broad category as “personality disorders and certain other nonpsychotic mental disorders.” DSM-II sexual deviations included sexual orientation disturbance (homosexuality), fetishism, pedophilia, transvestism, exhibitionism, voyeurism, sadism, masochism, and “other sexual deviation.”
The term paraphilias was introduced in DSM-III. The paraphilias were classified as psychosexual disorders, which included gender identity disorder, psychosexual dysfunctions, and ego-dystonic homosexuality. DSM-IV maintained the diagnostic classification of paraphilias. DSM-IV-TR moved transvestism from a disorder of gender identity to a paraphilia called transvestic fetishism.
The significant changes in DSM-5 include the change in nomenclature from “paraphilia” to “paraphilic disorder.” DSM-5 also introduced specifier terms such as “in remission,” and clarification between behavior and paraphilias.
DSM-5 classification
In DSM-5 the term paraphilia is defined as “any intense and persistent sexual interest other than sexual interest in genital stimulation or preparatory fondling with phenotypically normal, physiologically mature, consenting human partners.” Paraphilias, however, may not necessarily classify as “intense and persistent” but rather preferential sexual interests or sexual interests that are greater than nonparaphilic sexual interests. The addition of the word “disorder” to the classification of paraphilias is new to DSM-5.
Previous DSM classifications did not include the word “disorder.” The term “disorder” was specifically added to DSM-5 to indicate a paraphilia that is causing distress or impairment to the individual or a paraphilia whereby satisfaction entailed personal harm, or risk of harm, to others. This distinction was made in an effort to identify those sexual behaviors and interests that are of clinical significance.
With the change in nomenclature, some sexual behaviors may be classified as paraphilic but not disordered. In other words, some sexual behaviors may be outside normophilic interests but of no clinical significance.
Other significant changes to the paraphilias include the addition of specifiers to indicate the current status of the paraphilic interests and the grouping of disorders into classification schemes. The first group of disorders is classified as anomalous activity preferences. These anomalous activity preferences are subdivided into courtship disorders, voyeuristic disorder, exhibitionistic disorder, frotteuristic disorder, and algolagnic disorders, which involve pain and suffering (sexual masochism disorder and sexual sadism disorder).
The second group of disorders is classified as anomalous target preferences, which include pedophilic disorder, fetishistic disorder, and transvestic disorder. Paraphilia not otherwise specified has been replaced with specified paraphilic disorder and unspecified paraphilic disorder. The specifier “in a controlled environment” is used to refer to individuals living in institutional or other settings in which the object of sexual gratification is restricted. The specifier “in full remission” refers to the absence of distress or impairment in social, occupational, or other areas of function for at least 5 years.
Two new paraphilic disorders, paraphilic coercive disorder and hypersexual disorder, and one revision, pedophilic disorder to pedohebephilic disorder, were considered for inclusion in DSM-5. Paraphilic coercive disorder refers to a diagnostic category based on sexual arousal to coercion or non-consenting sexual behavior. Hypersexual disorder refers to an excessive level of sexual behavior or preoccupation that results in clinically significant impairment in functioning. Pedohebophilic disorder was coined to refer to sexual attraction to peripubescent children. The Paraphilia’s Sub-workgroup did not include any of these proposed changes, which suggests that the proposed changes did not satisfy the general consensus of the scientific community.
Role of psychiatrists
The management of sexual offenders in the US has largely been under the clinical expertise of psychologists. However, when the construct for civil commitment of sexually dangerous persons was enacted almost 20 years ago, psychiatrists, including the American Psychiatric Association, were in a position to become involved in sex offender management.
Although the role of psychiatrists in sexual offender management has been accepted by some, others have rejected the role of psychiatrists in this area, identifying a lack of training and experience as well as a lack of clarity as to what specifically psychiatrists can offer sexual offenders. The risk of committing future sexual offenses is lowered with the combination of biologic and psychologic treatments. More specifically, evidence-based practice supports the use of biologic treatment, namely antiandrogen and hormonal medications, in dangerous sexual offenders.1
The costs and consequences of sexual violence are vast. The best available research tells us that sexual violence victimization costs the US $450 billion annually.2 The answer to preventing sexual abuse is effective evaluation and treatment of sexual offenders. Psychiatrists are an integral part of this solution.
Only some individuals with paraphilic disorders commit sexual offenses. Studies vary but suggest that many individuals who meet criteria for paraphilic disorders do not act on their sexual orientation. Psychiatrists have a unique role in primary prevention by treating paraphilic disorders with the goal of preventing future sexual offenses.
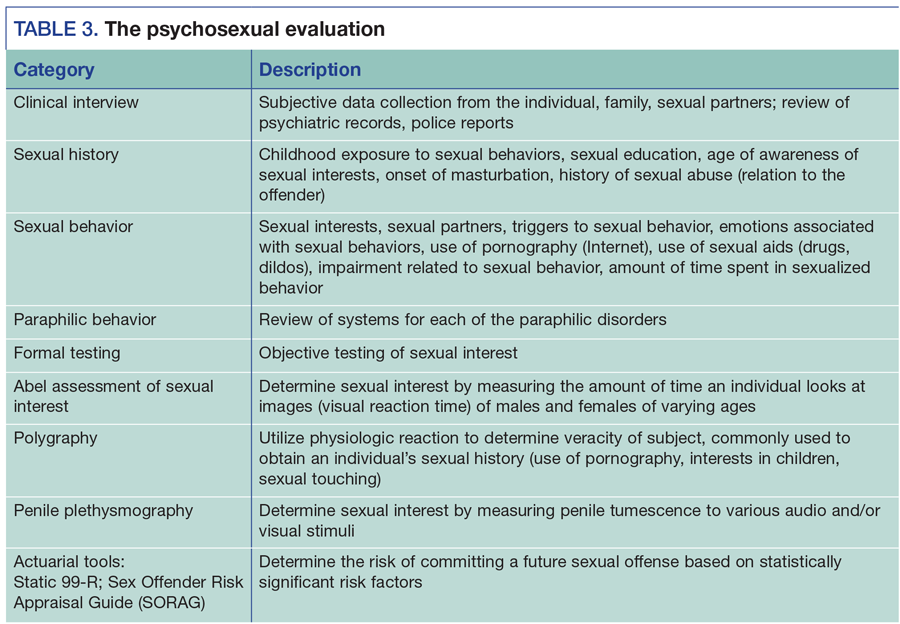
Research shows there is a high comorbidity of general psychiatric disorders in paraphilic sexual offenders.3 Axis I disorders including mood disorders, social anxiety disorder, autistic spectrum disorders, ADHD, and Axis II neurodevelopmental conditions such as intellectual disabilities (eg, fetal alcohol spectrum disorder) are psychopathologies reported as co-associated with paraphilic sexual offending.
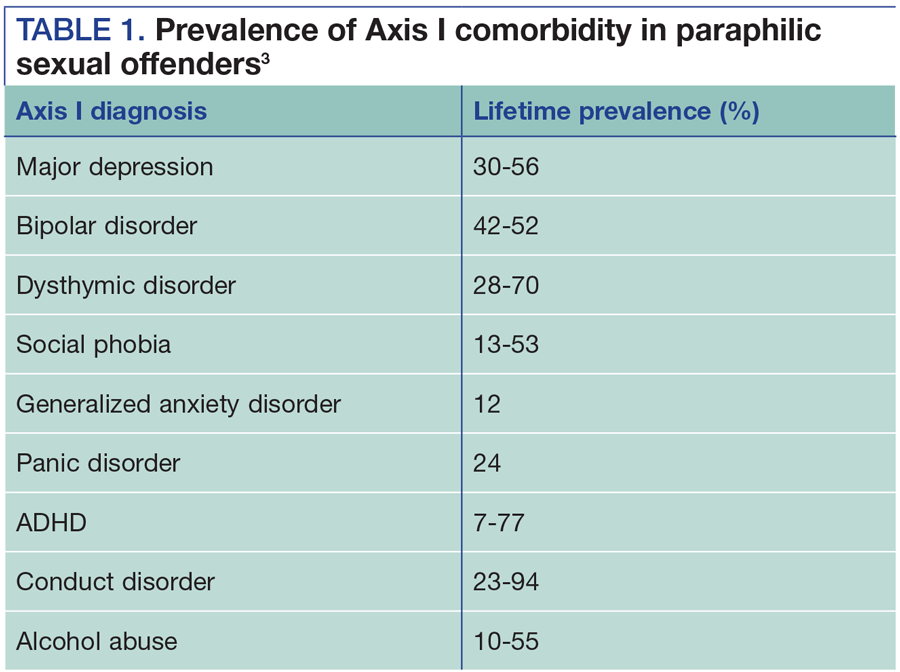
The concurrent psychiatric treatment of Axis I and Axis II comorbidities may reduce paraphilic behavior. Axis III conditions such as traumatic brain injury, temporal lobe epilepsy, and neurodegenerative conditions can present with paraphilic-like symptoms. The recognition of such medical conditions can lead to appropriate treatment. Psychiatrists can have an indirect role in decreasing sexual offending by adequately treating the comorbid, nonparaphilic disorder or treating the medical condition that presents as a paraphilia (Tables 1 and 2).
If order cheap cialis try my storefront you do not use the right manner of elimination then it can show various kinds of diseases in the reproductive system.
Psychosexual evaluation and treatment
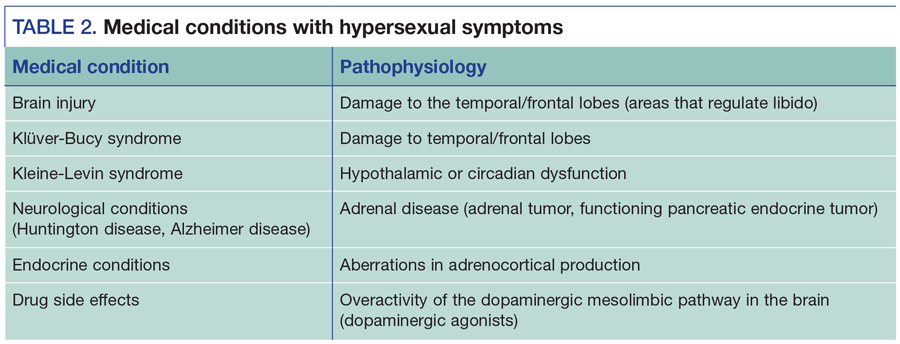
The etiology of paraphilias is unknown, but it is probably a learned behavior. Paraphilias occur primarily in males with an average onset between ages 8 and 12. They are a lifelong condition. Treatment is focused on decreasing the arousal to the deviant sexual behavior, rather than extinguishing the sexual orientation. The evaluation of an individual with problematic sexual behavior includes both a clinical (subjective) and testing (objective) component. The clinical interview includes a detailed sexual history, inquiring about childhood exposure to sexual acts, sexual partners, and sexual functioning such as masturbation pattern. A general medical and psychiatric history should be obtained to identify psychiatric comorbidity or medical conditions that mimic paraphilias (traumatic brain injuries, dopaminergic agents). Paraphilias may co-occur or change from one to another (“crossing-over”). The clinical interview should include a complete review of systems for each of the paraphilic disorders.
Individuals with paraphilic disorders or sexual offending may be unwilling to disclose their sexual interests. Objective testing to determine sexual interests include sexual history polygraphs, the Abel screen (associating visual reaction time with sexual interests), and the penile plethysmograph (measuring penile tumescence to sexual stimuli). Objective testing can be helpful in identifying problematic sexual orientation as well as measuring an individual’s response to treatment (Table 3).
Historically, psychotherapy was thought to be effective for the treatment of paraphilias and sexual offending. In the past decade, research has shown the most effective treatment of sexual offenders includes medication, behavioral therapy, social skills training, sex education, cognitive behavioral therapy, and monitoring with polygraph and penile plethysmograph.1
Forensic considerations
Civil commitment. Paraphilic disorders have not conventionally been viewed as major mental illnesses for the purposes of civil commitment to general psychiatric hospitals. Most general psychiatric units do not have expertise in the paraphilic disorders and as such do not offer inpatient treatment. Sexual offenders who have been adjudicated as sexually violent offenders or sexually dangerous offenders are civilly committed at designated facilities.
Mandated reporting. Psychiatrists who work with individuals with problematic sexual behaviors, namely pedophilia, should be comfortable with their role in mandated reporting. Psychiatrists are mandated to report suspected cases of child abuse or neglect. In order to be an effective clinician, psychiatrists who work with pedophilias must be comfortable identifying what clinical situations mandate reporting. Currently, California is the only state that mandates reporting of individuals engaged in child pornography.
Developing expertise. Currently, there are few psychiatrists trained in the area of paraphilic disorders. Most of the general psychiatric residencies and forensic fellowships do not provide clinical experience in this area. As a result, there remains a growing demand for psychiatrists with such expertise.
Psychiatrists who have an interest in the paraphilias may gain experience by working with an expert in the field. Although there are currently no paraphilia fellowship training programs, some experts in the field offer clinical rotations in the field. One way to familiarize yourself with such experts is to contact the Association for the Treatment of Sexual Abusers (ATSA) and inquire about state and local chapters. ATSA also provides awards and grants to individuals starting in the field.
One of the challenges of working in this area is the overlap of legal, social, political, and ethical considerations, which factor into the evaluation and treatment of sexual offenders. In my opinion, this overlap provides for a stimulating, diverse multidisciplinary approach to the treatment of patients.
The field of sex offender research has grown exponentially in the past 20 years. Today, a competent psychiatrist in this area must be familiar with the current evaluation and treatment guidelines, standard of care actuarial assessments, and sex offender laws in his or her jurisdiction.
DISCLOSURES
Dr. Sorrentino is Clinical Instructor at Harvard Medical School in Boston and Medical Director of the Institute for Sexual Wellness in Weymouth, MA. She reports no conflicts of interest concerning the subject matter of this article.
REFERENCES
1. Thibaut F, De La Barra F, Gordon H, et al. The World Federation of Societies of Biological Psychiatry Guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11:604-655.
2. National Institute of Justice. Victim costs and consequences: a new look. Washington, DC: US Department of Justice, Office of Justice Programs. https://www.ncjrs.gov/pdffiles/victcost.pdf. Accessed June 1, 2016.
3. Kafka, M. Axis I psychiatric disorders, paraphilic sexual offending and implications for pharmacological treatment. Israel J Psychiatry Relat Sci. 2012; 49:255-261.